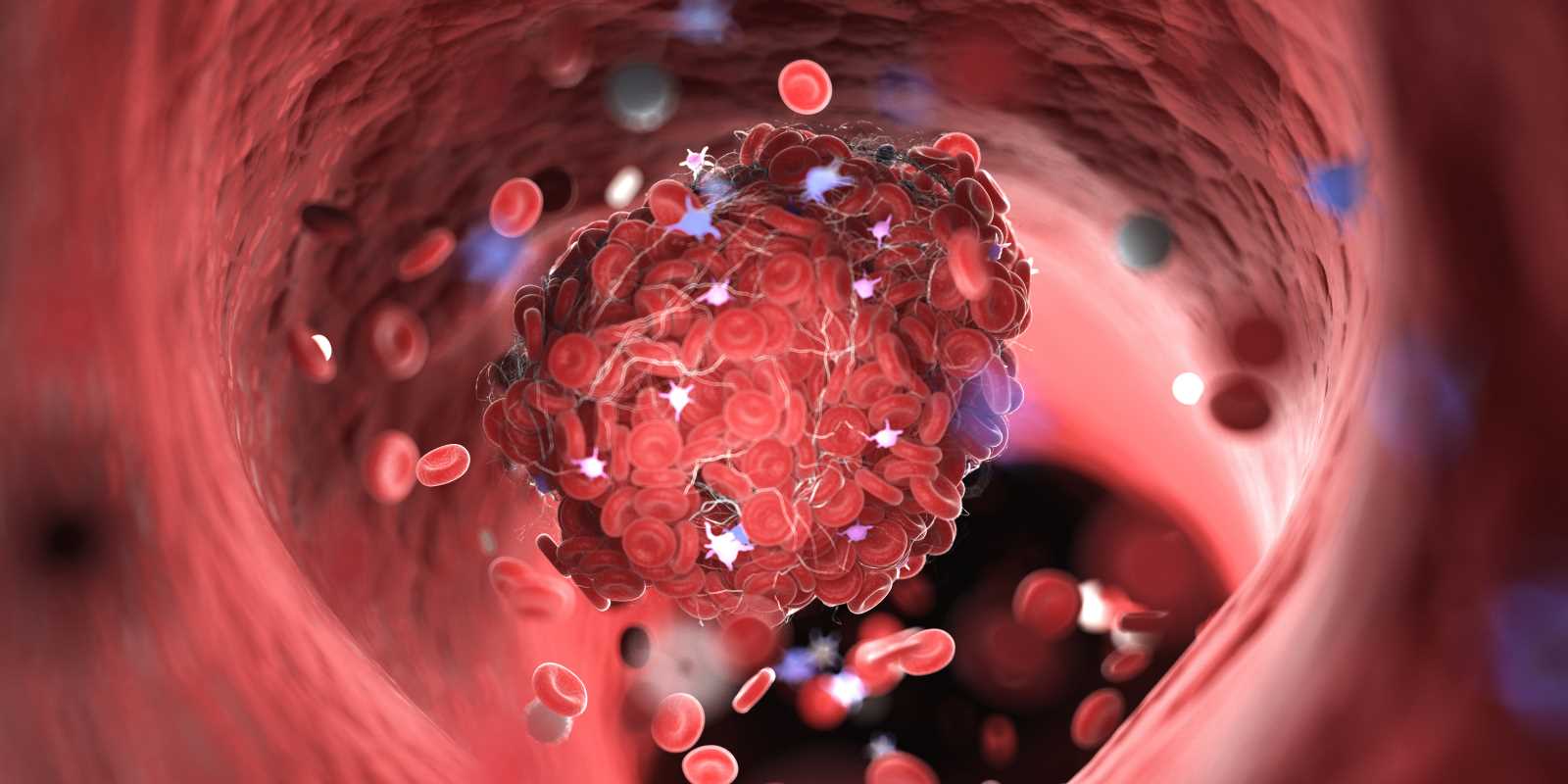
Blood clots are like nature’s bandages for your body. When you get a cut or injury, your blood forms clots to stop the bleeding and help you heal. But sometimes clots form in places they shouldn’t, like inside your veins or arteries. When this happens, it can lead to serious health problems, such as strokes, heart attacks, or deep vein thrombosis (DVT).
To treat or prevent these dangerous clots, doctors often prescribe anticoagulants. These medications, sometimes called blood thinners, don’t actually thin your blood. Instead, they make it harder for clots to form or grow. If you or someone you love is starting on anticoagulants, you might have questions. What do they do? Are they safe? How do they fit into a healthy routine? This guide will break it all down in simple terms so you can better understand how these meds work and how they’re used to manage blood clots.
What Are Anticoagulants?
Anticoagulants are a type of medication that helps stop your blood from clotting too easily. When your blood clots in the wrong place or at the wrong time, it can block the flow of blood to important areas in your body. For example, a clot in a vein in your leg could travel to your lungs, causing a potentially life-threatening condition called a pulmonary embolism (PE).
Anticoagulants don’t dissolve clots that already exist. Instead, they keep clots from getting bigger and help stop new ones from forming. This gives your body time to naturally break down the existing clot on its own. These meds are often prescribed for people who’ve had blood clots before or who are at high risk of developing them.
Common Conditions Treated with Anticoagulants
Anticoagulants are used to manage or prevent several health conditions. Here are some of the most common ones:
1. Deep Vein Thrombosis (DVT)
DVT occurs when a clot forms in a deep vein, usually in the legs. Symptoms might include swelling, pain, or redness, but sometimes there are no symptoms at all. If left untreated, a DVT can travel to the lungs and lead to a pulmonary embolism.
2. Pulmonary Embolism (PE)
A pulmonary embolism happens when a blood clot gets stuck in one of the blood vessels in your lungs. This can block blood flow, making it hard to breathe and causing chest pain. A PE can be life-threatening without quick treatment.
3. Stroke Prevention
Some strokes happen when a clot blocks blood flow to the brain (ischemic stroke). Anticoagulants are often prescribed to people at higher risk of strokes, such as those with atrial fibrillation (a type of irregular heartbeat).
4. Atrial Fibrillation (AFib)
Atrial fibrillation can cause blood to pool in your heart and increase the chances of clots forming. Taking anticoagulants can lower the risk of a clot traveling to your brain or other parts of your body.
5. Post-Surgery Clot Prevention
After certain surgeries, like hip or knee replacements, the risk of developing blood clots goes up. Anticoagulants are often used to reduce this risk during recovery.
Types of Anticoagulants
There are several kinds of anticoagulants, and each works in a slightly different way. Your doctor will choose the best option for you based on your condition, medical history, and lifestyle.
1. Warfarin (Brand Name: Coumadin)
Warfarin was one of the first anticoagulants and has been used for decades. It works by blocking vitamin K, which your body needs to make clotting proteins.
- Pros: Effective and well-studied.
- Cons: Requires regular blood tests to monitor its effects and careful attention to diet since vitamin K (found in foods like spinach and kale) can interfere with it.
2. Direct Oral Anticoagulants (DOACs)
DOACs are newer anticoagulants that are easier to manage because they don’t require regular blood tests like warfarin. They include drugs like rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa).
- Pros: Convenient, with fewer interactions with food or other medications.
- Cons: They might not be suitable for everyone, like patients with certain kidney problems or mechanical heart valves.
3. Heparin
Heparin is usually given through an injection, often in a hospital setting. It works quickly and is often used when an immediate effect is needed, such as during or shortly after surgery.
- Pros: Works fast and is effective for short-term use.
- Cons: Requires injections and close monitoring.
4. Low Molecular Weight Heparin (LMWH)
Similar to heparin, LMWH is also given as an injection. It’s commonly used during pregnancy or after surgery to reduce clot risk.
- Pros: Easier to use than regular heparin.
- Cons: Still requires injections, which might not be ideal for everyone.
Side Effects of Anticoagulants
Like all medications, anticoagulants come with some potential side effects. The most important one to be aware of is an increased risk of bleeding. Because these drugs slow down your blood’s ability to clot, even a small cut or injury might take longer to stop bleeding.
Here’s what to watch for while on anticoagulants:
- Easy bruising
- Nosebleeds that take longer to stop
- Bleeding gums when brushing your teeth
- Heavier-than-normal periods
- Blood in your urine or stool (this might look red or dark, like coffee grounds)
If you experience serious bleeding (like a deep cut that won’t stop or signs of internal bleeding, such as coughing up blood), get medical attention right away.
Living with Anticoagulants
If you’re starting anticoagulant therapy, adjusting to your new routine is important. Here are some tips to help:
1. Take Your Medication Exactly as Prescribed
Skipping doses or taking too much can make your blood too thin or not thin enough, increasing your risk of complications.
2. Watch for Signs of Bleeding
Be mindful of how your body reacts. Notify your doctor if you notice unusual bruising or bleeding.
3. Avoid Risky Activities
Because of the bleeding risk, try to avoid activities where you could get injured, like contact sports.
4. Inform Your Healthcare Providers
Always tell your dentist, surgeon, or any new healthcare provider that you’re taking anticoagulants. This helps them take necessary precautions.
5. Stay Consistent with Dietary Guidelines
If you’re on warfarin, try to eat a consistent amount of vitamin K-rich foods daily rather than completely avoiding them. Your doctor can help set up a plan based on your eating habits.
Questions to Ask Your Doctor
When starting on anticoagulants, open communication with your doctor is key. Here are some questions you might want to ask:
- Why are you prescribing this specific anticoagulant for me?
- What side effects should I watch for?
- Can I take this medication with my existing prescriptions or vitamins?
- Are there foods or drinks I need to avoid?
- How often will I need follow-up appointments or blood tests?
 (Image via
(Image via





